What is frozen shoulder?
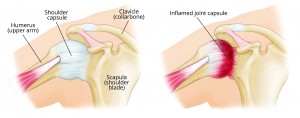
Frozen Shoulder, otherwise known as adhesive capsulitis, is an inflammatory condition causing pain and stiffness of the main shoulder joint (the gleno-humeral joint).
Causes
Adhesive capsulitis may occur following minor trauma to the shoulder joint (e.g. a mild strain), causing inflammation of the flexible lining of the joint capsule. The result is a thickening and tightening of the tissue, which subsequently limits shoulder movement in all ranges and results in pain.
Repetitive actions (e.g. throwing, racquet sports and swimming a single stroke in the pool) may also increase the risk.
Other risk factors that may influence the development of adhesive capsulitis include:
- Diabetes
- Heart disease
- Connective tissue disorders (e.g. Dupytren’s contracture)
Symptoms
Symptoms most often begin with several weeks of acute pain, followed by a period of disabling shoulder joint stiffness.
The affected ranges of shoulder movement initially include movement of the arm away from the body to the side (abduction of the shoulder) or to the front (flexion of the shoulder). In addition, rotation of the arm becomes problematic (e.g. brushing hair, fastening a bra, putting on a coat, removing a ticket at the car park barrier, closing the boot of the car, lying on the affected side in bed).
A typical adhesive capsulitis pattern consists of the following three phases:
Phase 1: FREEZING (the most painful phase, lasting between 2 and 10 months).
Phase 2: FROZEN (less painful but increasingly stiff, lasting between 4 and 12 months).
Phase 3: THAWING (gradually less pain and stiffness, over a varied period of time).
Prevalence
Adhesive capsulitis affects approximately 5% of the population. It is most prevalent in middle age (peaking between 40-60 years of age), affecting women slightly more than men.
Diagnosis
Commonly adhesive capsulitis is misdiagnosed as tendonitis of the shoulder muscle tendons, a muscular strain or tear, damage to the glenoid labour (cartilage cuff) of the shoulder joint and/or calcium deposits within the shoulder capsule and localised soft tissues.
Treatment
- Non-steroidal anti-inflammatories and pain killers to help reduce pain and inflammation.
- Prescription medication from the GP as required.
- Conservative manual therapy with an osteopath, aiming to reduce the local inflammation, to maximise the shoulder joint range of movement and to treat the surrounding (compensatory) regions.
- Steroid injections (in the initial stages).
- Hydrodilation (stretching of the joint capsule by injecting fluid into it).
- Surgery (manipulation under anaesthetic).
- Capsular release (using a radio-frequency probe to release the tight joint capsule).