Osteopathy, patellar tendonitis and marathon training
Introduction
Several of our patients at Woburn Osteopaths have started their training schedules for the impending London and Brighton Marathons in April 2020. We are so excited for them – particularly those seeking to beat that all important PB (personal best) & those aiming to complete their first ever 26.2 mile event (a runner never lets you forget that last punishing 0.2 miles)!
Is it therefore a coincidence that we are starting to see more and more overuse running injuries, in particular patellar tendonitis? We think not.
What is patellar tendonitis?
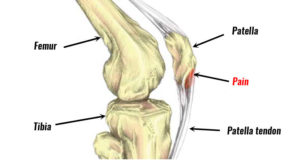
Patellar tendonitis is a common injury or inflammation of the tendon connecting the kneecap (the patella) to the large shinbone (the tibia). It is also known as Jumper’s Knee.
Causes
Patellar tendonitis is the result of repetitive stress on the knee, most often from overuse in sports and/or exercise. The repetitive stress on the knee creates micro tears in the tendon which, over time, inflame and weaken the tendon.
Symptoms
- Pain at the base of the patella, particularly when pressing it
- Some localised swelling and/or a burning sensation
- The base of the patella may appear larger and/or thicker than the uninjured side
- The onset of the pain is usually gradual and unspecific
- The pain may be sporadic, occurring only after sports and/or exercise activity
- As the tendon becomes more damaged, the pain can become progressively worse
- Aching and stiffness after exercise
- Kneeling down and/or getting up from a squat (when contracting the quadriceps muscles) can also be painful
Aggravating factors
- Tight leg muscles
- Weakness of the Vastus Medialis Oblique (VMO) muscle on the inside of the thigh (VMO keeps the patella on track, which in turn affects the direction of the forces through the patella tendon) and the calf muscles
- Leg length discrepancy
- Obesity
- Increasing running mileage too quickly
- Running shoes with insufficient shock absorption
- Hard playing surfaces
- History of associated injury
- Long periods of running
- Chronic diseases that weaken the tendon
How bad is my patellar tendonitis?
Symptoms are graded from 1 to 4 depending on the severity of the pain:
Grades
- Pain only after training
- Pain before and after training, pain eases once warmed-up
- Pain during training which limits performance
- Pain during everyday activities
Diagnosis
- Case history with your osteopath / GP / other manual therapist
- Physical examination, including active-resisted muscle testing and joint range of motion
- Imaging of the knee to determine if there’s any damage to the tendon or bone as well as to rule out an underlying fracture.
- X-ray examines the bone to determine whether there is a fracture or displacement of the patella
- MRI examines the tendon to highlight any damage to the associated soft tissues
- Ultrasound also examines the tendon to show any soft tissue damage
Complications
If patellar tendonitis progresses without an adequate management plan, it may lead to long-term damage of the patellar tendon and limited daily function.
It can be a tricky condition to treat, requiring a substantial period of rest and thorough treatment and rehabilitation. Enforced rest can be emotionally difficult, in particular for athletes.
If the injury is not looked after, the patient may require surgical intervention.
Treatment
Treatment depends on the severity of the injury.
Conservative measures to reduce pain, a period of controlled rest and stretching / strengthening the leg muscles are generally the first lines of treatment.
GPs may prescribe anti-inflammatories for short-term pain and inflammation reduction (e.g. ibuprofen, naproxen).
If the pain is severe a corticosteroid injection in the localised area may be administered. Some specialists are hesitant about a jab on the premise that it may also weaken the patellar tendon. It is therefore important to consider the associated risks before agreeing to a corticosteroid injection.
Rehabilitation
The goal of rehabilitation is to (1) reduce pain and inflammation and (2) stretch and strengthen the muscles of the leg and thigh.
If the pain is severe at rest, a brace and the use crutches is advisable for a while to avoid further damage to the patellar tendon. When the patient is relatively pain-free, rehabilitation can begin involving:
- Warm up
- Ice
- Manual therapy
- Stretching exercises
- Strengthening exercises
Some therapists may administer ultrasound and electrical stimulation to ease the knee pain. A knee brace or functional (kinesio) taping of your knee may help reduce pain during exercise by keeping the patella in situ.
A detailed rehabilitation programme should incorporate:
- Specific stretches for the thigh and calf
- Isometric exercises (joint angle and muscle length remain fixed during contractions) with the aim of relieving pain
- Eccentric exercises (e.g. squats performed on a decline board at a 25-degree angle)
- Flexibility exercises for the thigh and calf
Alternative treatments
A relatively new treatment is a platelet-rich plasma injection. This uses a concentration of platelets from the patient’s own blood to promote healing of the tendon.
Other alternative treatments under study include:
- Ultrasound-guided dry needling – this process makes small holes in the tendon, which has been found to relieve pain and facilitate healing
- Injections with polidocanol – aims at breaking up new blood vessels on the tendon, which are associated with pain
- High volume ultrasound-guided injections – this also aims at breaking up new blood vessels on the tendon
- Hyperthermia thermotherapy – this uses deep-tissue heating along with a cooling device on the skin surface to relieve pain
- Extracorporeal shockwave therapy – this has shown to reduce pain for up to two years
Surgery
Traditional surgery involves opening the knee to debride the patella and tendon. Arthroscopic (key hole) surgery is used for this procedure, which involves making four small incisions in the knee. It has a shorter recovery time than open surgery.
Recovery from surgery may vary. Some surgical protocols advise immobility in a cast after the operation. Another strategy involves an aggressive and immediate rehabilitation exercise programme.
For some athletes, patellar tendonitis may be chronic. For others, adequate rehabilitation can enable a return to normal functioning and sports. Recovery for mild injuries can be 1-month, while more severe injuries may require 6-8 months or more.
Important factors in recovery are:
- Committing to an adequate rehabilitation programme and exercising regularly
- A graded return to sports / exercise
- Respecting pain and resting accordingly
- Using anti-inflammatories and ice to help fluctuating pain