Osteopathy & Achilles tendonitis – advice and management
 What is Achilles tendinopathy?
What is Achilles tendinopathy?
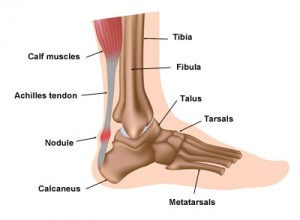
Tendons attach muscle to bone. The Achilles tendon is the thickest, largest and strongest tendon in the body. Located at the back of the lower leg, it attaches the two calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus), enabling us to to go on tiptoes or move forward when we walk, run and/or climb.
A tendinopathy occurs when a tendon is unable to adapt to the strain being placed upon it, leading to repetitive damage within the tendon fibres. Achilles tendinopathy (AT) involves irritation of the Achilles tendon, leading to increasing pain, swelling and stiffness at the back of the ankle / lower leg. AT occurs for a number of reasons.
Risk factors
AT is not simply the result of training too much.
- AT is a soft tissue injury affecting those who participate in recreational and/or competitive sports.
- AT can also occur in less active people.
- AT is seen in participants of sports with a high volume of running and jumping such as dance, gymnastics, football, tennis and badminton.
- AT is especially common in runners.
- AT is more common in men.
- AT is more common from the age of 30 onwards.
- AT is more common in people who are overweight.
- Diabetes increases the risk of developing AT.
- Tension, weakness and/or poor endurance strength of the calf muscles all contribute to AT.
- Poor stability around the hip/knee joints & stiffness of the foot and ankle joints add to AT.
Training errors
Certain aspects of exercise and training increase the risk of developing AT, such as:
- Increasing running mileage / training session duration too quickly (maximum 10% per week).
- Running at a too high an intensity.
- Excessive hill running.
- Old / poor quality footwear (trainers should be replaced after every 300-500 miles).
Common symptoms
The most common symptoms of AT include:
- Morning stiffness, which often eases after a few minutes of walking, but may last longer.
- Tenderness to touch or squeeze the Achilles tendon.
- A palpable thickening / lump within the fibres of the Achilles tendon.
- An audible clicking from the tendon when moving the foot and ankle.
- Varying levels of discomfort from the Achilles tendon, ranging from moderate to severe.
Treatments
There is no overnight cure for AT. The following list of treatments can offer relief from AT symptoms:
- Relative rest from aggravating activities, whilst maintaining levels of fitness via different forms of exercise such as swimming and cycling.
- Cool-packing the tendon with frozen peas in a pillow case (to avoid burning the skin) for a maximum of 20-minutes at a time up to 4 times a day or after exercise.
- Non-steroidal anti-inflammatories (e.g. ibuprofen) and/or paracetamol.
- Stretching the calf muscle complex (gastrocnemius and soleus).
- Osteopathy in conjunction with an eccentric exercise programme.
- Orthotics (shoe inserts) to support the arches of the foot.
- Autologous blood injections into the Achilles tendon to stimulate a healing response.
- Dry needling (Western acupuncture).
Eccentric exercise programme
The aim of an eccentric exercise programme is to gradually increase the stress going through the Achilles tendon in a controlled way. The exercises may take between 3 and 6 months to improve the symptoms of AT. Sometimes this may happen more quickly. Symptoms often worsen before they slowly improve, especially when progressing to each new phase of the exercise programme.
If you would like any advice or treatment for Achilles tendinopathy please do not hesitate to contact Woburn Osteopaths: 01525 290615.