Inflammation is part of the body’s defence mechanism and it plays an important role in the healing process.
When the body detects an intruder, it attempts to remove it via a biological response. The intruder could be a foreign body (e.g. a splinter), an irritant or a pathogen (e.g. bacteria, viruses and other organisms which cause infections).
Sometimes the body perceives its own cells and/or tissues to be harmful in error. This reaction can lead to autoimmune diseases such as Type 1 Diabetes. People with these conditions often have higher levels of inflammatory markers in their bodies.
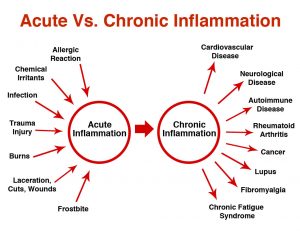
Types of Inflammation
(1) Acute inflammation
An injury or illness can involve acute (short-term) inflammation.
There are five key signs of acute inflammation:
- Pain: this may occur either continuously or when the affected area is touched.
- Redness: this happens because of an increase in the blood supply to the capillaries in the area.
- Loss of function: there may be difficulty in moving the affected area (e.g. a joint).
- Swelling: local oedema may develop if fluid builds up.
- Heat: increased blood flow may leave the affected area warm to the touch.
These signs are not always present as inflammation can be asymptomatic. Conversely, a person may also feel tired, generally unwell and have a temperature.
Symptoms of acute inflammation last up to 72-hours. Thereafter sub-acute inflammation lasts 2-6 weeks.
(2) Chronic inflammation
Chronic inflammation may continue for months and/or years. It has associations with various diseases, such as:
- Diabetes
- Cardiovascular disease
- Osteoarthritis
- Rheumatoid arthritis
- Allergies / intolerances
- Psoriasis
- Chronic obstructive pulmonary disease (COPD)
The symptoms will depend on the disease, but they may include pain and fatigue.
Measurements
When inflammation is present in the body, there will be higher levels of biomarkers are detected. An example such a substance is CRP (C-reactive protein). If a doctor wants to test for inflammatory markers, they may assess CRP levels in the blood. CRP levels tend to be higher in older people and those with conditions such as cancer and obesity.
Causes
Inflammation occurs when a physical factor triggers an immune reaction. Inflammation does not necessarily mean that there is an infection, but an infection can cause inflammation.
Acute inflammation can result from exposure to a substance (e.g. a splinter, dust, an insect bite or sting), injury and/or infection.
When the body detects damage or pathogens, the immune system triggers a number of responses:
- Body tissues accumulate plasma proteins, leading to a build up of fluid and subsequent swelling.
- Neutrophils – a type of white blood cell (leukocyte) containing molecules that can help to fight the pathogens- are released, which move towards the affected area.
- Small blood vessels dilate to enable leukocytes and plasma proteins to reach the injury site more efficiently.
Signs of acute inflammation may appear within hours or days, depending on the cause. How they develop and how long they last will depend on the cause, which part of the body they affect, and individual factors. In some instances signs of acute inflammation may become severe with little or no warning.
Chronic inflammation can develop if a person has:
- Sensitivity to an external trigger that should not be present, often resulting in an allergy.
- Long-term, low-level exposure to an irritant (e.g. an industrial chemical).
Factors that may increase the risk of chronic inflammation include:
- Older age
- Obesity
- Diet rich in unhealthy fats and added sugar
- Smoking
- Stress
- Sleep disturbance
Autoimmune disorders occur when the immune system mistakenly attacks normal healthy tissues (e.g. psoriasis).
Auto-inflammatory diseases are the result of a genetic factor affecting the way the immune system functions (e.g. Behçet’s disease).
Persistent acute inflammation is where a person does not fully recover from acute inflammation, leading to chronic inflammation.
Long-term diseases associated with inflammation include:
- Asthma
- Tuberculosis
- Rheumatoid arthritis
- Inflammatory bowel disease (Ulcerative Colitis / Chron’s Disease)
- Sinusitis
- Hepatitis
Treatment
Treatment of inflammation will depend on the cause and severity. It is essential to identify and manage inflammation and related diseases to prevent further complications (e.g. sepsis).
Acute inflammation
A doctor may prescribe treatment to remove the cause of inflammation, manage symptoms, or both.
For a bacterial or fungal infection, for example, they may prescribe antibiotics or antifungal treatment.
Here are some treatments specifically for treating inflammation:
Nonsteroidal anti-inflammatory drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) will not remove the cause of inflammation, but they can help relieve pain, swelling, fever, and other symptoms. They do this by countering an enzyme that contributes to inflammation.
Examples of NSAIDs include naproxen, ibuprofen, and aspirin. These are available to purchase online or over the counter. People should check first with a doctor or pharmacist to ensure they make the right choice.
People should only use NSAIDs long term if a doctor recommends them, as they can have adverse effects. Aspirin is not suitable for children.
Pain relief: Acetaminophen, including paracetamol or Tylenol, can relieve pain but does not reduce inflammation. These drugs allow the inflammation to continue its role in healing.
Corticosteroids
Corticosteroids, such as cortisol, are a type of steroid hormone. They affect various mechanisms involved in inflammation.
Corticosteroids can help manage a range of conditions, including:
- Arthritis
- Temporal arteritis
- Dermatitis
- Inflammatory bowel disease (IBD)
- Systemic lupus
- Hepatitis
- Asthma
- Allergic reactions
They are available as pills, injections, in an inhaler, or as creams or ointments.
Long-term use of corticosteroids can be harmful. A doctor can advise on their risks and benefits.
Treatment for diseases that involve long-term inflammation will depend on the condition.
Some drugs act to repress the body’s immune reactions. These can help relieve symptoms of rheumatoid arthritis, psoriasis, and other similar autoimmune reactions. However, they can also leave a person’s body less able to fight an infection if it occurs.
People who have undergone transplant surgery also need to take immunosuppressant drugs to prevent their bodies from rejecting the new organ. They, too, need to take extra care to avoid exposure to infections.
Herbs for inflammation
Various herbal supplements may help manage inflammation, including but not limited to:
Ginger: People have long used ginger to treat dyspepsia, constipation, colic and other gastrointestinal problems, as well as rheumatoid arthritis pain.
Turmeric: Curcumin, the main ingredient in turmeric, may have benefits for arthritis, Alzheimer’s disease and some other inflammatory conditions.
Nutrition
Some foods contain nutrients that may help reduce inflammation, including but not limited to:
- Olive oil
- High fibre foods
- Tomatoes
- Nuts, such as walnuts and almonds
- Leafy greens, including spinach and kale
- Oily fish, such as salmon and mackerel
- Fruit, including blueberries and oranges
Studies have suggested that people with high levels of CRP may be less likely to follow a diet that is rich in fresh products and healthy oils, such as the Mediterranean diet.
The following foods may aggravate inflammation:
- Fried foods
- Highly processed foods
- Foods and drinks with added sugar
- Red meat
- Unhealthy fats, such as saturated and trans fats
Diet alone will not control inflammation, but making suitable choices may help prevent it from getting worse!